Donor Alan Bernstein shares how Nazareth Home saved his life

Alan Bernstein, a former military policeman in the Army and someone considered reasonably physically fit, started a downward health spiral in January 2021 after contracting COVID-19. That would begin a very difficult period in his life where he developed pneumonia, spent five long months on a ventilator, and was unconscious for a period of time. Alan recalls feeling “like being twisted into a pretzel” after he lost 51 lbs. and “being in terrible pain.” That’s when he wanted to throw in the towel. He’d received care in multiple healthcare facilities, had lost much of his hope, and began saying goodbye to loved ones. But, Dr. Jignesh Desai told Harriette Friedlander, Alan’s wife, that he could control the pain and keep Alan going.
With Dr. Desai’s news, Harriette wasn’t ready to stop fighting. Over time, Alan began to see some health improvements and found himself in inpatient rehab at another facility. After two weeks, the facility said that was as far as they could take him; they could do no more.
Harriette knew in her heart he wasn’t ready to come home and thought of Nazareth Home based on great things she’d heard from friends in the community.
“Nazareth Home was just where I wanted him to be,” she said. So, in June 2021, Alan came to the Recovery to Home program at Nazareth Home’s Highlands Campus for several months of inpatient therapy.
“There’s no reason I should be alive today,” said Alan. “To take care of sick old people and still have a good sense of humor, the staff were angels. The rehab team was just incredible. And I loved being able to decide what I wanted to eat, sit where I wanted at lunch, and have meal partners that I could laugh with. We were all having challenges and it was great to be able to bond and laugh with others.”
While receiving therapy at Nazareth Home, Alan developed a special bond with the therapy program director, Matt Tuley. Alan smiled when sharing, “Matt and I developed a relationship beyond a patient and therapist. He was like a little brother to me.”
 Alan was able to joyously return home in September 2021 and received home health care, respite care, and even equine therapy from Allison Wheaton at Summit Equestrian Center in Fort Wayne, Indiana, through the VA. Alan hadn’t been on a horse in more than 20 years. No one could have imagined that he would go from the dire, bedridden state he was in to now riding a horse, doing Pilates, and cruising around the world. Friends see him and remark about his miracle of progress.
Alan was able to joyously return home in September 2021 and received home health care, respite care, and even equine therapy from Allison Wheaton at Summit Equestrian Center in Fort Wayne, Indiana, through the VA. Alan hadn’t been on a horse in more than 20 years. No one could have imagined that he would go from the dire, bedridden state he was in to now riding a horse, doing Pilates, and cruising around the world. Friends see him and remark about his miracle of progress.
Alan credits Nazareth Home with saving his life and is now a donor to the Nazareth Homes Foundation, helping to support the patients, programs, and team members in our ministry.
“Very simply, Nazareth Home kept me alive. After all you did for me, how could I not offer something back? Nazareth Home went above and beyond for me,” he said.



 Louisville often calls itself the home of the aging care and aging innovation industry. We gathered three top professionals in the field to talk about the state of business and how they are navigating through major challenges in workforce, funding and attitudes toward senior populations. Joining this sponsored content conversation were
Louisville often calls itself the home of the aging care and aging innovation industry. We gathered three top professionals in the field to talk about the state of business and how they are navigating through major challenges in workforce, funding and attitudes toward senior populations. Joining this sponsored content conversation were 

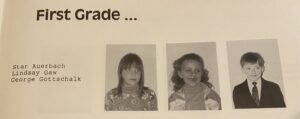
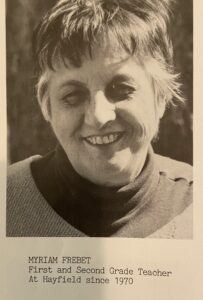 As the two of them reminisced together over old school yearbooks, Myriam turned to Lindsay and said with a smile, “You certainly were a wonderful first grader.”
As the two of them reminisced together over old school yearbooks, Myriam turned to Lindsay and said with a smile, “You certainly were a wonderful first grader.”